The sad but true statistic remains that over 250,000 preventable deaths occur across the US healthcare system each year. A little more math shows that almost 700 individuals every day succumb to some sort of medical error – what the healthcare system refers to as an “adverse event.” In addressing the magnitude of this data, leaders across the healthcare ecosystem continue working to identify and quantify a wide range of solutions, but remain frustrated by the complexity of the system they work within and the lack of standardization – and transparency – across the products and procedures that intersect at the patient point of care.
Many believe – incorrectly – that the electronic medical record (EMR) is the answer. However, despite the best intentions of clinicians, researchers and healthcare data scientists, EMR can’t deliver effective root cause analysis and development of solutions to prevent medical errors that lead to “never events” because of its retrospective, “post-event” usage. Lack of standardization, transparency and traceability of care processes mean the healthcare industry at large can’t deliver the detail necessary to document and address the risk to patients in real time that can inform clinicians to help prevent adverse events.
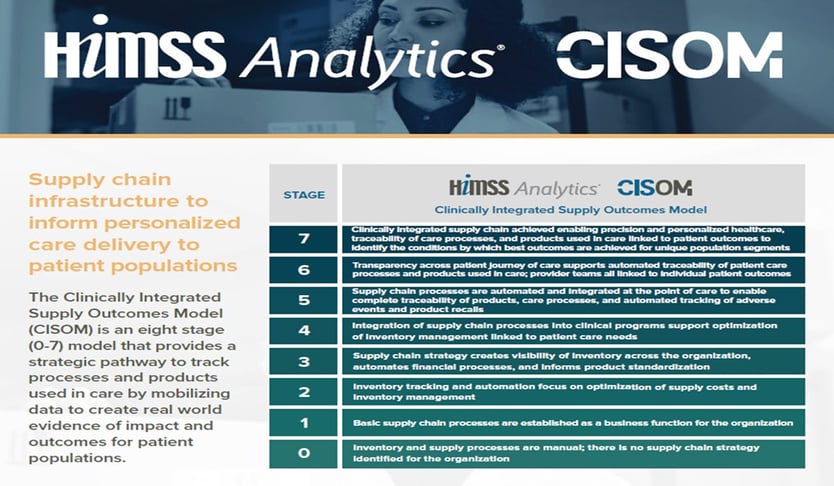
In a significant move toward real-time preventative intervention (vs. current post-event analytics), HIMSS has developed the Clinically Integrated Supply Outcomes Model (CISOM), an eight-stage model for building a supply chain infrastructure that delivers important safety and quality benefits. Organizations that adopt and implement the CISOM approach by focusing on four key areas of their supply chain (automation, clinical integration, predictive data analytics, governance and leadership) are more likely to improve their clinical supply chain management, increase the performance of their care delivery capabilities and reduce the instance of adverse events within their system.
So why does this matter to RTLS? Nearly all the “never events” experienced by healthcare systems can be mitigated or eliminated through system transparency using the CISOM approach to deliver automated tracking and traceability at the patient point of care. Proper design and implementation of a comprehensive real-time tracking and tracing methodology for patients, products, medications and devices can dramatically reduce adverse and/or never events. Patient location, infant security and patient wander/elopement are some instances where a thoughtful and thorough RTLS solution can make a measurable difference in any hospital or clinical setting.
Does your facility approach intervention and prevention of “never events” this way? If not, let IMS help your organization build an infrastructure that brings the value of a transparent supply chain to the front line of patient safety.
Footnotes: https://www.himssanalytics.org/news/cisom-deep-dive-focus-areas